Doctors spend a lot of time entering clinical notes into patient charts at the end of the day. But a new artificial intelligence program could do away with this practice for good. MaineHealth recently announced it is using AI to automatically record conversations between doctors and their patients during a check-up or follow-up visit. The software then transcribes the information and enters the most important details into the patient’s chart, so doctors don’t have to spend as much time entering info by hand.
Dr. Daniel Nigrin, chief information officer at MaineHealth, says the technology should help reduce physician burnout by helping providers spend more time with patients.
“This saves physicians what we call ‘pajama time,’ when they finish their work after hours, and the patient gets the full attention from the physician and full eye contact,” he said.
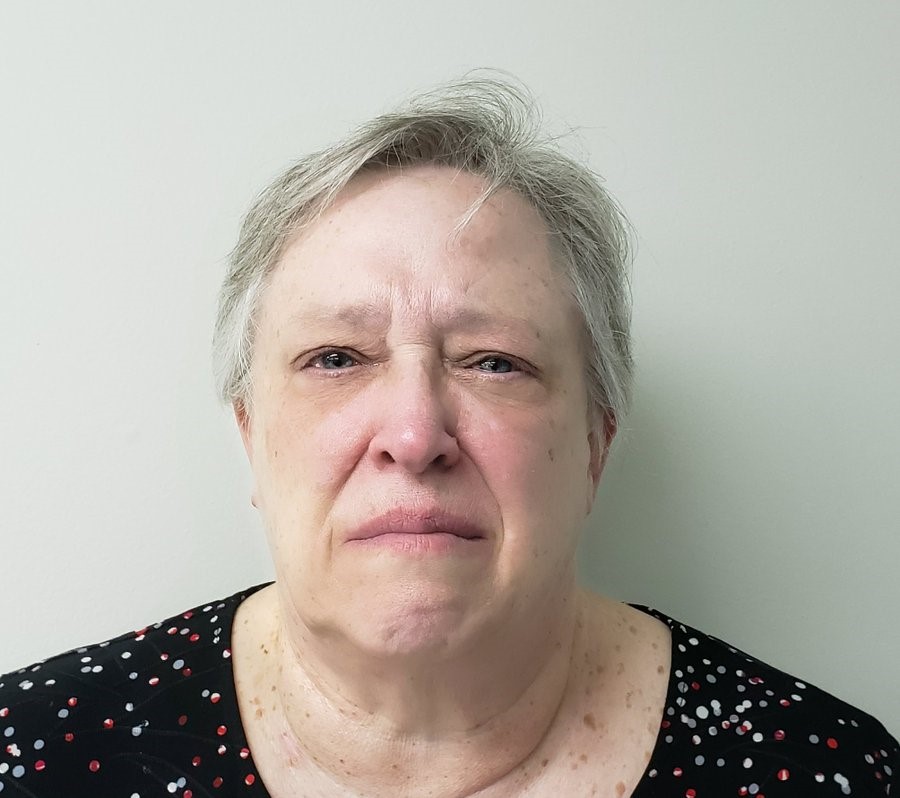
Deborah Vaughan, a patient at the hospital, said she appreciates being able to look her doctor in the eye while talking about her health. Her regular doctor, Dr. Rebecca Hemphill, used the AI app during her last two medical appointments at MaineHealth.
“The main thing is she can concentrate more on a patient and not be typing on a keyboard and glancing over,” Vaughan said. “It feels more like my needs are being met. And there’s not as much pressure on the doctor.”
But is the software accurate?
Experts say the AI is able to point out the most important information from the meeting, so both parties can refer back to it at a later date.
Vaughan’s doctor even offered to let her check the clinical notes at the end of the session and they were accurate.
MaineHealth is the first healthcare facility in the state to incorporate this kind of artificial intelligence.
Hemphill said the tool has been a huge help at work. It helps her pay more attention to her patients, many of whom just want to be heard. “We end up doing what we went into medicine for,” she said.
The AI is part of a four-month pilot program at the health system. It’s being used at 25 physician offices in Portland and Southern Maine. The company says it is still evaluating the potential costs and benefits of the app. Hemphill declined to mention the price tag but said she hopes it will be worth it in the future.
Providence Health, a national health system, pays $8,000 to $10,000 per year per doctor to license the same AI software, according to recent reporting.
“Nobody went into medicine to write notes or fill out insurance authorization forms,” said J. Scott Smitherman, chief medical information officer at Providence Health. He added that medical payers now require so much documentation related to patients that “it’s almost an arms race.”
The AI is sold under the name Dragon Ambient Experience or DAX. It was designed by a Massachusetts company called Nuance Communications, which is owned by Microsoft, the same company the recently purchased OpenAI, which runs Chat-GPT.
Hemphill said it does more than just transcribe human speech. “It understands the principles of what is being discussed, not just the words,” she explained.
The app will transcribe the notes in around four hours. It also keeps the patient’s data secure.
She also added that all of her patients appear comfortable with the idea of her using the technology. No one has refused the AI during a clinical visit, but some people may have an issue with being recorded, especially when talking about their health. She said it may not be the right fit for every physician, but it has benefited her practice enormously and the app is only getting smarter every day.
“You are training the system with your voice and information, and it trains you to be more organized,” she said.
Other providers are worried about the app leaving out crucial information that could be essential to patient care.
“The major concerns I would have here is I’m not sure the computer would be smart enough to know what is important [enough] to pull out into the note,” said Dr. Shravani Durbhakula, a pain physician and anesthesiologist at the Johns Hopkins School of Medicine, which doesn’t use tools like DAX to automate clinical notes. “You could miss critical information.”
For example, she said the program will add a note if a patient experiences endocrine dysfunction, but it may code it as the result of a testosterone deficiency rather than an opioid-induced deficiency, which is a key piece of information that could affect the care they receive. This information would never make it into the system, which could hurt patient outcomes.
“That could continue to get missed in other portions of the evaluation process,” she said.