There’s a new weight loss drug on the market that’s quickly surging in popularity. It’s called semaglutide and is sold under the brand names Ozempic, Wegovy, and Rybelsus. The drug is an antidiabetic medication that’s used as an appetite suppressant in individuals looking to lose weight. The FDA has approved semaglutide for once-daily use in those struggling with obesity. It works by activating the glucagon-like peptide-1 (GLP-1) hormone that regulates blood sugar levels, which increases the production of insulin to lower blood sugar levels.
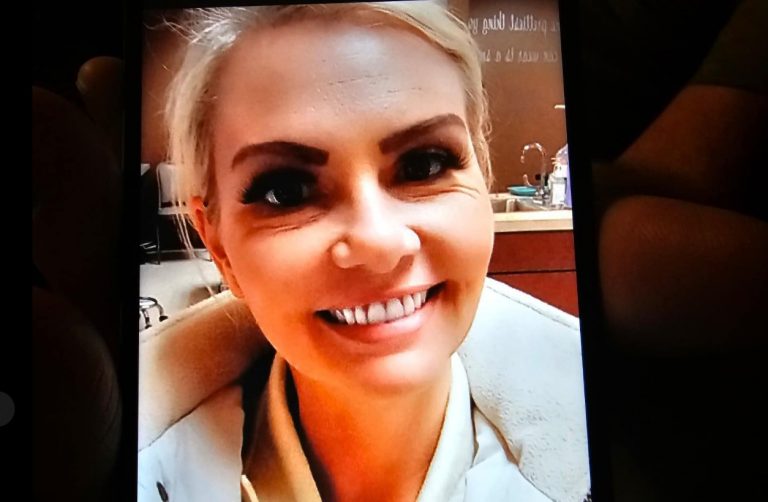
Meredith Schorr, a nurse, recently took Ozempic for weight loss after gaining an extra fifty pounds during the COVID-19 pandemic. The long hours of the job, stressful working conditions, and the medication she was taking for PTSD contributed to her poor diet and lack of exercise.
“I was pretty uncomfortable with the new weight that I had gained because it wasn’t where I normally sat. I didn’t feel healthy, I was restricted in doing exercise,” said Schorr. Before the pandemic, she said she was fit and healthy.
That’s when her friend recommended that she try a type 2 diabetes drug known as Ozempic. This particular form of semaglutide is injected in the thigh, arm, or stomach. Schorr decided to ask a nurse practitioner who specializes in weight loss about the medication.
“She basically made it clear to me that I can use this drug as a tool to help me lose weight, and garner the motivation to improve my lifestyle habits,” she explains. “She made sure that I knew that the drug wasn’t just a crutch to rely on, I had to make lifestyle changes as well.”
Schorr received a prescription for the drug, which cost around $150 per month with insurance.
Within 24 hours, she started experiencing side effects, including stomach pains, excess gas, cramping, constipation, and intense nausea.
“I seemed to have more severe side effects than most, but I later learned how to combat that with all sorts of non-pharmacological interventions, and also had to be prescribed Zofran,” she continues. “And then all of a sudden I started losing weight pretty drastically.”
She ended up losing 50 pounds in 11 months while taking the drug. It even helped her fit into her old wedding dress. But she made the decision to stop using the drug in January of this year because she wanted to start a family.
“I’m young and I’d rather not be on this medication for a long time. Plus, it’s expensive,” she adds.
But some health experts have warned that it’s easy for patients to regain the weight they’ve lost after going off the medication.
Schorr felt additional side-effects for a few weeks after stopping the drug. “Around that five-to-six-week mark, I began to feel super hungry, and almost ravenous for a little bit,” Schorr explains.
Two months later, she had regained 10 lbs. of the original 50 she had lost. But she was determined not to let her progress slip away.
“I was super hungry all of a sudden,” Schorr says. “So, after that phase, I was able to kind of see, ‘Oh, I gained 10 lbs. I don’t want to lose any progress that I had made.’ That’s the time where I tried to focus on healthier eating, choosing better snacks than what I may have in the past, making those conscientious choices to have a healthier lifestyle and diet, and that seems to have helped.”
The weight gain helped her realize that she needed to do more to maintain her new figure. “I worried about the side effects and readjustment just as much as I would worry with any other medication,” she continues. “There’s risks and benefits to every medication, so I just knew that a healthier lifestyle and habits was going to greatly benefit me.”
The medication has come under fire as of late as researchers learn more about the side effects, including possible muscle loss, but Schorr said she wouldn’t have been able to lose as much weight as she did without Ozempic.
“I feel like [Ozempic] has been so vilified lately but it was a really great tool for me and really changed my life,” she says. “Physically, I’ve been doing really well. I’ve been exercising so much more than I used to, eating right. I feel a lot more comfortable in my own skin. I feel really grateful.”
Ania Jastreboff, an obesity medicine physician scientist at Yale, said most people need to keep taking the medication to keep the weight off they’ve already lost.
“Not everybody needs the highest dose, but if you want to maintain the weight reduction that you achieved, you have to continue taking the medication,” Jastreboff explained. “The reason for that is because obesity is a chronic disease,” she says, adding that the drugs have not been tested for people who do not have type 2 diabetes or chronic obesity.
“If you have a patient who has high blood pressure, they have hypertension, and you start them on an antihypertensive medication, and their blood pressure improves, what would happen if you stopped that medication? Well, their blood pressure would go back up — and we’re not surprised. It’s the same with anti-obesity medications,” she says.