Living with diabetes and varicose veins can be tough. Diabetes affects how your body handles sugar, and varicose veins are swollen, twisted veins in your legs. Together, they can cause a lot of discomfort and serious health problems if not managed well. This article will share tips on managing both conditions and keeping your legs healthy and strong.
Importance of Managing Diabetes and Varicose Veins Together
Managing these conditions together is crucial because they can exacerbate each other. Bad blood circulation due to varicose veins can worsen diabetes symptoms, while uncontrolled diabetes can increase the risk of developing varicose veins. By understanding their interplay, you can take proactive steps to manage both conditions effectively.
Understanding Varicose Veins
Varicose veins are swollen, enlarged veins that often appear dark blue or purple. They occur when valves in the veins that prevent blood from flowing backward fail, causing blood to pool and veins to enlarge. Varicose veins occur in the legs due to the pressure of walking and standing.
Symptoms
Common symptoms of varicose veins include:
– Aching
– Swelling
– Heavy feeling in the legs
Pay special attention to any of these symptoms in your legs and visit a Varicose vein doctor if you notice changes.
Complications
Varicose veins can lead to complications when untreated, such as:
– Skin ulcers
– Blood clots
– Chronic venous insufficiency
In these conditions, blood flow in the veins is inadequate.
Causes of Varicose Veins
Some chronic conditions can increase the risk, like diabetes. Other factors can contribute to the development of varicose veins, including:
– Age
– Genetics
– Obesity
– Pregnancy
– Prolonged standing or sitting
Understanding Diabetes
Diabetes is a long-term health issue marked by elevated levels of sugar in the blood, known as glucose. It occurs when the body either doesn’t produce enough insulin or can’t effectively use the insulin it does produce. Insulin is a hormone that assists in the entry of glucose into cells to use energy.
Types of Diabetes
There are three main types of diabetes:
– Type 1: an autoimmune condition where our body attacks insulin-producing cells.
– Type 2: more common and occurs when our body resists insulin.
– Gestational diabetes: it appears during pregnancy and usually goes away after childbirth but increases the risk of developing Type 2 diabetes later.
How Diabetes Affects Your Body
Diabetes affects various organs and systems in the body, including:
– The cardiovascular system
– Kidneys
– Eyes
– Nerves
High blood sugar levels damage nerves and veins over time, leading to complications such as:
– Heart disease
– Kidney failure
– Vision problems
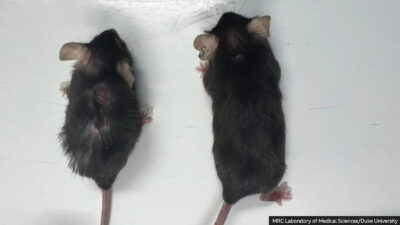
The Link Between Diabetes and Varicose Veins
Diabetes can worsen varicose veins due to its impact on blood circulation and blood vessel health. High blood sugar levels lead to bad circulation, exacerbating the swelling and discomfort associated with varicose veins.
Common risk factors for both conditions include obesity, a sedentary lifestyle, and a family history of either diabetes or varicose veins. Additionally, aging and hormonal changes can increase the risk of developing both conditions.
Lifestyle Changes for Managing Diabetes and Varicose Veins
There are certain habits you can change to cope with diabetes and varicose veins. From dietary changes to physical activity, there is always something you can do to improve your health.
Foods to Include
Having a good diet rich in lean proteins, fiber, and healthy fats can help manage diabetes and varicose veins. Include foods like:
– Whole grains
– Fruits
– Vegetables
– Nuts
They improve blood sugar control and promote good circulation.
Foods to Avoid
Avoiding some foods can prevent spikes in blood sugar and reduce fluid retention. It is beneficial for managing both conditions to avoid foods like:
– Sugary snacks
– Excessive salt
Exercise and Physical Activity
Regular exercise helps improve insulin sensitivity and control blood sugar levels. Aerobic exercises like walking, swimming, and cycling are particularly beneficial for people with diabetes.
Some exercises can improve leg strength and circulation, such as:
– Leg lifts
– Calf raises
– Yoga
You can reduce the symptoms by practicing them regularly. Regular movement prevents blood from pooling in the veins.
Maintaining a healthy weight is key for handling both diabetes and varicose veins. Excess weight adds extra pressure on your legs and can worsen both conditions. Regular physical activity and a good diet will help you maintain an ideal weight.
Medical Treatments and Interventions
If you’re having these conditions, it’s important to know your options for a medical treatment or intervention. Here are some of the main ones.
Medications for Diabetes
Medications are important for managing diabetes. There are different types, including insulin and oral medications. Insulin is required by individuals with Type 1 diabetes and occasionally by individuals with Type 2 diabetes. Oral medications like metformin help control blood sugar by improving how your body uses or makes insulin. Adhering to your doctor’s guidance and consistently monitoring your blood sugar levels is crucial to ensuring effective treatment.
Treatments for Varicose Veins
Varicose veins may cause discomfort, yet there are numerous methods available to address them. One way is to make lifestyle changes. Move more and avoid standing or sitting for too long. Compression stockings can also help. They reduce swelling and improve blood flow in your legs.
In more severe cases, medical procedures might be needed. Sclerotherapy entails the injection of a solution into the veins to make them disappear. Laser treatments use strong light to close off smaller veins. Sometimes, surgery is needed to remove or close veins. Your doctor will tell you what the best treatment for you is.
Combined Treatment Approaches
Handling diabetes and varicose veins usually needs a mix of methods. This means dealing with both problems at the same time through changes in lifestyle, medicines, and sometimes surgery. For example, exercising regularly and eating well can control blood sugar levels and make blood flow better, which helps both diabetes and varicose veins.
Sometimes, you might need to work closely with a healthcare team that includes:
– Your primary doctor
– A nutritionist
– A vascular specialist
Working together with your healthcare providers ensures that both conditions are managed well, preventing problems and making life better. Regular check-ups and talking openly with your healthcare providers are important to stay on the right path with your treatment.
Conclusion
Managing diabetes and varicose veins needs a comprehensive approach, including medical treatments, lifestyle changes, and regular monitoring. By adopting healthy habits, seeking appropriate medical care, and staying informed, you can effectively manage both conditions and maintain healthy legs. Remember, a positive attitude and consistency are essential. Stay proactive, and don’t hesitate to seek support when needed.