Uncategorized
“Supermodel Granny” Drug Extends Lifespan in Lab Animals
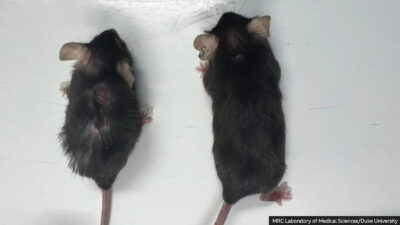
A drug has been shown to extend the lifespan of laboratory mice by nearly 25%, offering promising implications for human aging. Treated mice, ...