Doctors and providers use medical algorithms and equations when assessing a patient’s risk of illness or disease and recommending treatment. However, many of these programs use race as part of the analytics process. In fact, they may alter their recommendations or findings once the patient’s race is added into the system, a trend known as race correction.
But critics say these “corrections” tend to be misleading – if not dangerous – to patients of color.
What Is Race Correction?
Race correction is defined as the use of a patient’s race in a scientific equation that then influences how they are treated. That means some diagnostic algorithms and risk predictor tools will essentially adjust or “correct” their results based on the person’s race.
There are many examples of this. The New England Journal of Medicine flagged 13 programs and risk predictor tools for using race correction in the article “Hidden in Plain Sight”.
One is known as the Vaginal Birth After Cesarean calculator. Doctors and providers use this tool to determine the likelihood of a healthy pregnancy after a prior C-section. Black and hispanic patients tend to get a lower score on the program, which means the doctor is more likely to recommend a C-section, but that usually comes with increased risk of blood loss, infection, and longer recovery times.
The American Heart Association’s Get with the Guidelines–Heart Failure tool is another. Doctors use this to predict in-hospital mortality rates among patients with acute heart failure. Clinicians are advised to use this risk stratification to guide decisions regarding initiating medical therapy. The New England Journal of Medicine found that the program adds 3 points to the risk score if the patient is identified as non-black, thus increasing their risk of estimated probability of death. This often puts black and hispanic patients at a disadvantage. The race correction regards black patients as lower risk and may raise the threshold for using clinical resources for black patients.
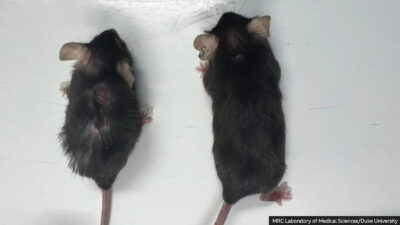
The Organ Procurement and Transplantation Network: Kidney Donor Risk Index (KDRI) is used to estimate the risk of donor kidney graft failure when allocating kidneys to transplant patients. The tool looks at several factors, including age, race, hypertension, diabetes. Researchers noted increases in the predicted risk of kidney graft failure if the potential donor is identified as African American.
The Lasting Scars of Racism
According to Carolyn Roberts, historian of medicine and biology at Yale University, these ideas can be traced back to slavery, when the medical industry experimented on black slaves only to perfect them before using them on white people. This led to the myth that black and white bodies are inherently different, most notably like Dr. Samuel Cartwright’s claim in 1851 that black people have weaker lungs.
These myths linger on today. A 2016 study asked white medical students about these alleged differences between black and white bodies. Forty perent of first-year medical students and 25% of residents said they believed black people have thicker skin, and 7% of all students and residents surveyed said black people have less sensitive nerve endings. These providers were also less likely to accurately prescribe medication for black patients.
Dorothy Roberts, a professor of law and sociology at the University of Pennsylvania, says the industry’s focus on race is doing more harm than good. For starters, race isn’t a biological category. It’s a social one.
“It’s based on this idea that human beings are naturally divided into these big groups called races. But that’s not what race is. Race is a completely invented social category. The very idea that human beings are divided into races is a made-up idea,” Roberts said.
Ancestry is biological, however, but providers don’t usually have the tools to accurately characterize a patient’s ancestral history.
Naomi Nkinsi was just one of five black medical students at the University of Washington when she discovered that providers often only have two options when using these diagnostic tools, including “black” and “other”. She was learning how to use eGFR equations that measure a patient’s kidney function.
“It was really shocking to me,” says Nkinsi, now getting her master’s degree in public health, “to come into school and see that not only is there interpersonal racism between patients and physicians…there’s actually racism built into the very algorithms that we use.”
Getting Rid of Racial Bias in Medical Algorithms
Medical student Carina Seah agrees. “You can be half black and half white in this country and you are black. You can be a quarter black in this country — if you have dark skin, you are black,” she says.
Nkinsi believes providers have to make split-second decisions regarding the patient’s ancestral history. “You have to ask, how black is black enough? It also puts the blame on the patient, and it puts the blame on the race itself. Like being black is inherently the cause of these diseases,” Nkinsi says.
Nkinsi and Seah are both focused on getting rid of these myths in medical algorithms, but students are often made to defer to doctors that have been practicing for years.
Seah even started an online petition and collected 1,600 signatures asking hospitals to remove the race correction from their eGFR programs. Researchers from Brigham and Women’s Hospital and Penn Medicine estimated up to one in every three black patients with kidney disease would have been reclassified if race correction wasn’t applied in earlier calculations, with a quarter being recategorized to stage 4 CKD (Chronic Kidney Disease).
Some argue that simply removing the race correction would lead to a knee-jerk reaction in the medical field as providers quickly change how they categorize patients of color. When removing race from the eGFR program, more black patients would likely qualify for specialists, but the downside would be that fewer black patients would qualify for a kidney transplant.
The leaders of both the National Kidney Foundation and the American Society of Nephrology recently announced that race shouldn’t be included in the eGFR equation.